Mobile team reintegration-rehabilitation: An activity outside. Results of 3 years of functioning to the Pole Saint-Helier
A Duruflé1, C Le Meur1, P Gallien1, C Lozach1, MP Reillon1, N Clerc1, M Jambou1, B Nicolas1
Abstract
Many mobile teams were created over the past decade in various medical specialties including physical medicine and rehabilitation.
The Pole Saint Helier has created a mobile team of reintegration - rehabilitation (EM2R) in December 2012 with support from the Regional Health Agency of Brittany. It operates on the health territory No. 5 of Brittany near people experiencing neurological disability. Its main mission is to implement the necessary devices to facilitate the home return of people hospitalized after a neurological event or maintaining to home people with neurological disorders.
The number of supported annual is about 200. People with brain lesions account for 2/3 of the population, mean age 60 years, with a high degree of dependence. The complexity of the patients become clearer with a minimum of two professionals involved by patient. Occupational therapy represents the majority of requests for intervention. New activities have emerged: supported to people with brain tumor, collaborations with palliative mobile teams and home hospital, formation and education of caregivers.
This activity outside is an alternative to the PMR care offer in link especially with the recommendations of the French Society of Physical Medicine and Rehabilitation and High Autority of Health on the organization of care pathway of stroke.
Introduction
Over the last decade, many mobile teams have been created in the health sector in France in various medical specialties including geriatrics, palliative care and psychiatry. Similarly, as part of an alternative to the cares’ possibilities usually offered in the rehabilitation sector, the physical medicine and rehabilitation (PMR) have also been concerned by the creation of mobile teams. This way of accompany is linked with the recommendations of the French Society of Physical Medicine and Rehabilitation which advocate the early discharge of patients after a stroke1. On the other hand, the creation of rehabilitation mobile teams at a scale of a health territory as part of the organization of stroke pathway is also highlighted in Appendix 9 of the report of the High Authority of Health2.
In France, numerous experiences exist with different ways to operate (mobile teams focused on a network, a care sector, at the patient home or in a hospital), and a variable composition depending on the territories and the missions. In general, mobile intervention teams of rehabilitation meet one or more of these missions: allow patients to go back to their home environment as fast as possible which contributes to the fluidity of care course, facilitate the discharge of patients from acute care services so these services can take care of patients who require specialized technical platform, be a support for home care services and professionals by the organization, coordination and providing additional expertise, establish a relay between the health, social medicine and home. Although most of these missions seem admitted by all, there is no consensus today at the national level on their mode of operation and in particular on their vocation to provide the care or not. Internationally, there is the action of these teams of early supported discharge (ESD) with a focus mainly on the stroke literature3,4,5,6 with a recent review of the literature Cochrane has shown the value of ESD (which include three types of care activities in France : inpatient, home hospitalization and mobile teams) including the length of hospital stay, independence and home support to 6 months, satisfaction and access to extended activities of daily living3.
Return of experience
The mobile team of reintegration - rehabilitation (EM2R) to the Pole Saint Helier started in December 2012 thanks to the support from the Regional Health Agency (ARS) of Brittany. Its main objective is to answer the need for fluidity of the course of care of the patients under 75 years with neurological diseases on the health care area No. 5 of Brittany.
The operational team is made with physical and rehabilitation doctors, a psychologist, two occupational therapists, a social worker.
The main missions of the EM2R are to enable the patient to recover its usual environment of life as soon as possible and be a support for institutions (health and medico-social), home care professionals or services in terms of inputs of complementary skills. This in the objective to implement devices necessary for the sustainability of home support or for make more fluid the network of management of patients with neurological disability.
Its field of intervention joins in the course of care of the patients with a neurological disability: in acute care services, then on rehabilitation care and finally at home. The EM2R can be asked by home or care services professionals: doctor, general practitioner, paramedics ... Support depend on the demand and needs identified at the first meeting.
Since the establishment of the EM2R, its activity has been increasing with a quickly reached objective of 200 interventions a year. The reasons for the request were mainly the support needs occupational therapy taken (home visit and/ or assessment needs). The average age of persons in care is about 60 years. Our target population for interventions is now defined as: 2/3 of the care population have brain damage (Chart 1) about is its origin with a high handicap level (54 % have a physical dependence more than 12 over 16 and 38 % have a relational dependence more than 5 over 8 in 2015) estimated by a dependence scale (common scale autonomy – dependence and French program medicalization of information systems)7.
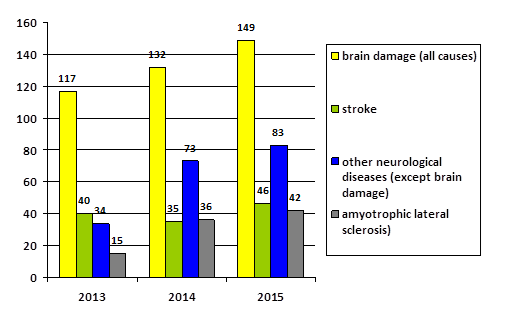
Figure 1: Type of diseases supported
Interventions are multiple and adapted depending on the initial request and the objectives decided with the patient. It concerns for example: home improvement, implementations of technical assistance or a service to provide assistance, psychological or social support, medical evaluation in PMR … The support is short (the median of duration of support is of 55 days in 2015) and multidisciplinary with a minimum of two professionals involved. Interventions are mostly Occupational Therapy. The average number of trips varies depending on pathologies and we see that the number of trips is higher for interventions on people with amyotrophic lateral sclerosis and multiple sclerosis. (Chart 2) Indeed, it is two chronic and evolutionary neurological pathologies which justify longer interventions and necessary adaptations with regard to the possible functional degradation.
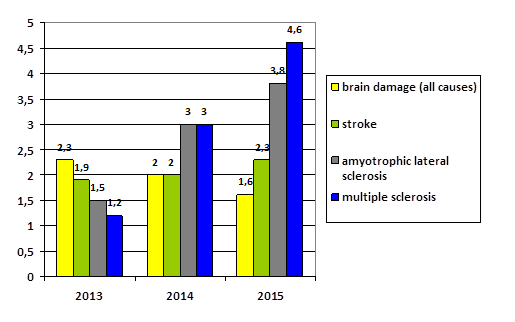
Figure 2: Average number of trips by disease
The main diseases concerned by our support are stroke and amyotrophic lateral sclerosis. (chart 1) Regarding to stroke, half of the interventions just followed hospitalization (post-hospital coordination). This support requires that hospital teams make use of EM2R to coordinate care at the discharge of acute care services. It requires a change in the hospital staff behavior and it is not yet a common practice today. Other cares are focused on the home and the sustainability of the ageing in place. The needs are variable and mainly occupational therapy (home facilities, technical assistance counseling, positioning, training of caregivers to technical transfer ...). Regarding to amyotrophic lateral sclerosis (ALS), these people have specific needs in terms of access to care especially occupational therapy and counseling since the beginning of the disease. Due to the evolving nature of the disease, interventions must be quick and it is in this context that the EM2R interventions comes in, with these individuals to meet their needs wich are evolving over time (sometimes quickly). This activity required the development of new collaborations in terms of a possible relay with specialized partners (reference centers ALS, palliative mobile teams, home medical care, departmental home for disables...) and in terms of collaborations, in a trustful relationship with the association for ALS and with the resellers of medical equipment in the different sectors.
To conclude, after these three first years of operation, we believe that rehabilitation mobile teams are a real alternative to care provision on the health area, building the support in a care course complementary of the on already existing (inpatient, day hospitalization, home hospitalization rehabilitation care). We are also convinced of the need to educate, train caregivers but also professionals in an accompanying common goal of people suffering from neurological disability at home on time of ambulatory care turn promoted by statutory texts in France. Our practices are sometimes changed because we work at patients’ homes with an essential collaboration with stakeholders at home and the use of new technologies such as telemedicine, innovative tool that allows us to save time, given extended territory of interventions. Finally, we have no indicator of efficiency of our activity except the follow-up of the satisfaction of the patients which is good (8,9 on 10 in 2016). We chose to measure as indicator of efficiency, the number of hours dedicated by the natural carvigers by means of their family before and after our interventions. Indeed, today, there is no modelling of rehabilitation mobile teams in the national level in France. The comparison to other existing mobile teams is thus difficult and the choice of our quality indicators and thus the efficiency will be to precise in the future.
References
- Orientation of stroke patients - Recommendations - Expert Conference with public hearing organized by the French Society of Physical Medicine and Rehabilitation (SOFMER), the French Society of Neuro Vascular (SFNV) and the French Society of Geriatrics and Gerontology ( SFGG) - Mulhouse October 22, 2008: www.sofmer.com
- Compared to Madame Minister: The prevention and management of stroke - Appendix 9 - The mobile team of rehabilitation and recovery across a health territory (support staff and coordination) : www.sante.gouv.fr
- Fearon P, Langhorne P. Services for reducing duration of hospital care for acute stroke patients. Cochrane Database of Systematic Reviews. 2012; 9: 1-97.
- Hofstad et al. Early supported discharge after stroke in Bergen ESD Stroke Bergen three and six months results of a randomised controlled trial comparing two early supported discharge schemes with treatment as usual. BMC Neurology. 2014; 14: 239.
- Taule T et al. Ability in daily activities after early supported discharge models of stroke rehabilitation. Scandinavian Journal of Occupational Therapy. 2015; 22: 355–365.
- Fischer et al. A Consensus on Stroke Early Supported Discharge. Stroke. 2011; 42: 1392-1397.
- Common scale autonomy – dependence and french program medicalization of information systems : http://www.atih.sante.fr/sites/default/files/public/content/1097/guidegcap.pdf
